| • What is Uveitis? |
| • What Causes Uveitis? |
| • Types of Uveitis |
| • Symptoms of Uveitis |
| • Treatment Strategies |
| • FAQs |
What Is Uveitis?
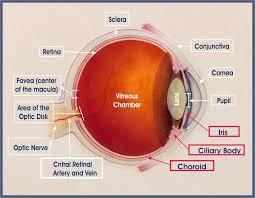 Uveitis is an inflammation of the uvea, which is made up of the: Iris (the coloured part of the eye), the Ciliary body (behind the iris and forms fluid inside the eye), and the Choroid (the vascular lining below the retina). Together, these form the middle layer of the eye between the retina and the sclera (white of the eye).It can also lead to inflammation in the adjacent areas, like the retina and fluid in the back of the eye (called vitreous).
Uveitis is an inflammation of the uvea, which is made up of the: Iris (the coloured part of the eye), the Ciliary body (behind the iris and forms fluid inside the eye), and the Choroid (the vascular lining below the retina). Together, these form the middle layer of the eye between the retina and the sclera (white of the eye).It can also lead to inflammation in the adjacent areas, like the retina and fluid in the back of the eye (called vitreous).
The uvea contains many blood vessels — the veins, arteries and capillaries — that carry blood to and from the eye. Because the uvea nourishes many important parts of the eye (such as the retina), inflammation of the uvea can damage your sight.
| • Systemic inflammatory diseases; |
| • A result of injury to the eye; or |
| • It may be associated with infection caused by virus, bacteria, fungus or a parasite. |
Types Of Uveitis
Uveitis can be of four types, depending upon the location of the inflammation.
There are several types of uveitis, defined by the part of the eye where it occurs.
| • Iritis or Anterior Uveitis affects the front of your eye. This is the most common type of uveitis. Iritis usually develops suddenly and is commonly associated with redness, watering, decreased vision, pain in the eye and photophobia or intense discomfort while looking at light. Some types of anterior uveitis can be chronic or recurrent. | 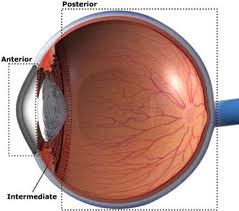 |
| • Pars planitis or Intermediate uveitis affects the middle or intermediate region of the eye. The patient usually sees black spots in front of the eye. There may be loss of vision due to fluid accumulation in the central area of the retina. The disease goes through cycles of getting better, then worse. |
|
| • Posterior uveitis affects the back parts of your eye. Posterior uveitis can develop slowly and often lasts for many years. The inflammation may affect the retina, choroid (posterior or back part of the middle layer) or both. The inflammation may be localized at several places, or even widely spread. Patients usually complain of poor vision, or the absence of central or peripheral vision. The eye may appear normal or there may be little inflammation in the front. | |
| • Panuveitis occurs when all layers of the uvea are inflamed. It often causes a distinct blurring of the vision with varying degrees of pain and redness. | |
Symptoms of Uveitis
Uveitis may develop suddenly with eye redness and pain, or with a painless blurring of vision. In addition, other symptoms of uveitis may include light sensitivity, blurred vision, decreased vision and floaters. There may also be a whitish area (called a hypopyon) obscuring the lower part of the iris.
Diagnosis of Uveitis
A careful eye examination by an ophthalmologist is extremely important when symptoms occur. Inflammation inside the eye can permanently affect sight or even lead to blindness if it is not treated.
Your ophthalmologist will examine the inside of your eye. He or she may order blood tests, skin tests or X-rays to help make the diagnosis.
Since uveitis can be associated with disease in other parts of the body, your ophthalmologist will want to know about your overall health. He or she may want to consult with your primary care physician or other medical specialists. However, in approximately 40 to 60 percent of cases, no associated disease can be identified.
| • Relief of pain and discomfort (where present) |
| • To prevent sight loss due to the disease or its complications |
| • To treat the cause of the disease where possible |
| • If you have a "red eye" that does not clear up quickly, contact your ophthalmologist. |
| • Uveitis is a serious eye condition that may scar the eye. It needs to be treated as soon as possible. Eyedrops, especially corticosteroids and pupil dilators, can reduce inflammation and pain. For more severe inflammation, oral medication or injections may be necessary. |
| • Even though there may not be a permanent cure for Uveitis, each attack can be treated, depending upon the cause, severity and location of the inflammation. The treatment may include eye drops, injections under the eye or oral medication. These drugs have potential side effects, but they are often not serious and their effects are reversible, once treatment is discontinued |
| • Glaucoma (increased pressure in the eye); |
| • Cataract (clouding of the eye's natural lens); |
| • Neovascularization (growth of new, abnormal blood vessels); or |
| • Damage to the retina, including retinal detachment, damage to the optic nerve or both. |
It is important to maintain regular follow-up by your treating ophthalmologist in order to monitor medications as well as progression of the disease. Because of the serious complications which may occur as a result of uveitis, an ongoing partnership between patient and ophthalmologist greatly increases long-term success.
Can Uveitis recur?
Yes, in many cases Uveitis can recur. The frequency and severity of the attacks is however, unpredictable. Consult your ophthalmologist as soon as you notice any signs of recurrence; this will make the treatment simpler and lead to a quicker resolution of Uveitis.
What are the likely complications?
Patients with Uveitis can develop complications like cataract, glaucoma, i.e., raised intraocular pressure (pressure of the eye, similar to blood pressure) and macular edema (fluid accumulation in the central part of the retina). This can lead to reduced vision. Such complications can be managed medically or surgically once the inflammation is controlled.
Can Uveitis lead to loss of vision?
Uveitis can lead to loss of vision if not managed properly. However, with modern diagnostic methods, better medication and surgical techniques, the prognosis for most patients is very good. It is critical that the disease is identified early and treated properly. It is also important for patients with uveitis to get their eyes checked periodically, even if there are no symptoms.
What you should know?
You must realize that every case of Uveitis is different - your case may not be exactly like any of the types described here. Do not hesitate to ask your doctor for further information.
We all have heard of double edged swords. Having two sharpened edges made it easy for the warriors to cut using either of the blades. However it also added to risk of hurting themselves. Did you know that your body also wields a similar sword? It is called inflammation, the reaction of your body aimed to eliminate harmful stimuli like germs, damaged cells or irritants. This comes with the risk of severe damage to your own tissues.
What is expected outcome? (Prognosis)
Most attacks usually get resolved in a few days to weeks after proper treatment. Recurrence is also commonly seen.
Inflammation involving the back of your eye usually takes a longer time to heal than that in the front part of your eye.
Inflammation due to posterior uveitis may last for years, sometimes even causing permanent damage to vision despite treatment.
What will happen to my eyes (prognosis)?
This varies considerably, but there is a growing confidence, especially with the newer drug treatments, that the eyesight can be stabilised over the long term. Uveitis as a disease should be regarded as incurable in the sense that it may never completely go away, but that is not to say that it cannot be controlled.
Why follow-up is more important in uveitis?
Regular follow-up is must in uveitis, as it can be a vision threatening. The treatment includes stronger drugs and so careful follow up is mandatory to avoid iatrogenic complications.
© Aggarwal Eye Hospital |
Site designed by Rainbow Web |